Release time :2023-12-28
Source:support@yingchitech.com
Scan:1012
Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd.
Post Traumatic Stress Disorder (PTSD) is a mental disorder that delays the onset and persists for a long time after experiencing or witnessing one or more actual deaths, or receiving death, serious injury, or various threats. Acute symptoms of PTSD, including persistent invasive recall, avoidance of trauma-related stimuli, negative cognitive and emotional changes, excessive arousal, and hyperalertness to traumatic cues, are latent and heterogeneous, greatly increasing the difficulty of diagnosis and treatment. Current drug treatments for PTSD are not very effective, resulting in at least one-third of patients experiencing no relief from their symptoms. Neurostimulation therapy, particularly the use of transcranial magnetic stimulation (TMS), has proven to be an effective tool for the treatment of PTSD.
In 2023, Professor Yang Qun's team from the Air Force Military Medical University teamed up with Xijing Hospital explored the effectiveness of intermittent theta burst stimulation (iTBS) mode and traditional repetitive transcranial magnetic stimulation (rTMS) in the treatment of post-traumatic stress disorder, and published the relevant results "Effects of intermittent theta-burst transcranial magnetic stimulation on post-traumatic stress disorder symptoms: A randomized controlled trial" in the journal Psychiatry Research (IF=11.3, 2023)


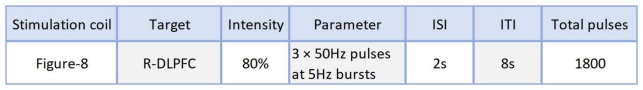
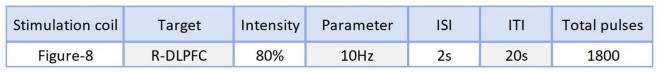
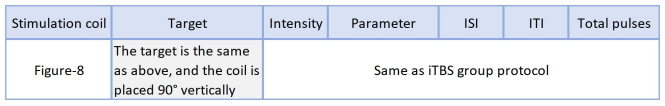
Seventy-five participants aged between 18 and 55 who had a score of at least 50 on the PTSD Cheeklist-Civilian Version (PCL-C) were selected. Participants were randomized in a 1:1:1 ratio to receive rTMS (n=25), iTBS (n=25) or sham stimulation group (n=25), and received 15 transcranial magnetic stimulation treatments for three consecutive weeks ( Monday to Friday, once a day). There were no significant differences in gender, age, and years of education between the three groups of patients. The trial stimulus package is as follows:
The PTSD Cheeklist-Civilian Version (PCL-C), which asks subjects to rate, on a five-point scale, how disturbed they civilian are by problems and complaints in the past month. 1 "not at all," 2 "a little bit," 3 "moderately," 4 "quite a bit," and 5 "extremely." The total score of each item (17 to 85) was accumulated, and the higher the score, the more likely PTSD was to occur.
Posttraumatic GrowthInventory (PTGI), which includes 21 items in 5 dimensions including new possibility, interpersonal relationship, personal strength, spiritual change and appreciation of life, is scored on 6 Likert scales. The higher the score, the higher the level of post-traumatic growth.

There were 22 cases in iTBS group, 20 cases in rTMS group and 21 cases in sham stimulation group. Demographic and clinical variables before intervention (T1) (gender, age, education, education level, PTSD, and PTGI scores) were not statistically significant between the three groups.
At the end of the overall intervention (T2), the average PCL-C score decreased from 67.86 to 39.68 in the iTBS group, from 65.21 to 39.13 in the rTMS group, and from 67.66 to 59.66 to 59.09 in the sham stimulation group. One month after the intervention ended (T3), the average total PCL-C scores further dropped to 31.86, 35.47 and 43.61 respectively. At the end of the overall intervention (T2), the average PTGI score increased from 52.31 to 72.77 in the iTBS group, from 49.47 to 72.95 in the rTMS group, and from 49.14 to 58.47 in the sham stimulation group.
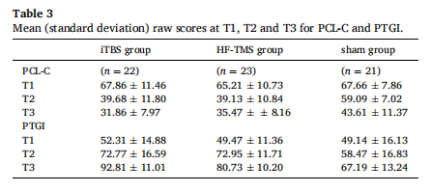
In addition, one month after the intervention ended (T3), the LSD-t test showed that subjects in both treatment groups responded significantly better than the sham stimulation group. The average difference in PCL-C total score between the iTBS group and the sham stimulation group was 10.32, and between the rTMS group and the sham stimulation group was 10.18. The average difference in PTGI total score between the iTBS group and the sham stimulation group was 14.36, and the PTGI between the rTMS group and the sham stimulation group was 9.454. There was no significant difference in efficacy between the iTBS group and rTMS group. The average difference in PCL-C between the iTBS group and the rTMS group was 0.13, and the average difference in PTGI between the iTBS group and the rTMS group was 4.911.
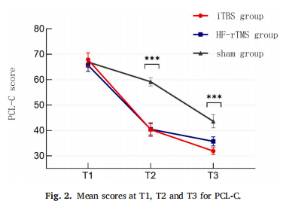
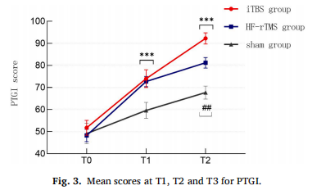

The PCL-C and PTGI scores of the iTBS and rTMS groups were significantly different from those of the sham stimulation group. There were no significant differences in PCL-C and PTGI scores between the two active treatment groups. iTBS treatment has a shorter duration and can effectively improve PTSD symptoms, with no significant difference in efficacy from rTMS.
Previous studies have found that the use of high-frequency stimulation of the right dorsolateral prefrontal cortex (DLPFC) is the most effective way to treat PTSD, and the mechanism may be that TMS can regulate the excitability of the prefrontal and hippocampus regions, thereby improving the brain function of the corresponding regions. In addition, TMS can regulate the level of brain-derived neurotrophic factor, promote the formation of neurons and synaptic plasticity, as well as accelerate the metabolism of the stimulated site of the hippocampus. In a way, it can reverse the abnormal pathological and molecular changes that occur in the brains of PTSD patients. With the development of neuroimaging in recent years, changes in functional connections between brain regions have been found in individuals with PTSD symptoms, such as enhanced functional connections between the amygdala and hippocampus, greater activity in the amygdala, and greater activation in the right frontal lobe when processing trtrauma related stimuli. TMS can partially regulate areas such as the amygdala by creating functional connections, which can enhance fear elimination, among other things. TMS promotes the elimination of fear, which may be one of the important reasons for the improvement of PTSD symptoms.
This is the first randomized controlled clinical trial to compare iTBS treatment with 10 Hz rTMS and sham stimulation, validating that both iTBS and standard 10 Hz rTMS are effective in reducing PTSD symptoms. Compared with standard 10 Hz rTMS, iTBS treats PTSD with similar efficacy and acceptability, while iTBS treatment duration is much shorter. Therefore, iTBS has the advantages of increasing machine application efficiency, reducing waiting times, and potentially reducing costs, and is worthy of promotion as an intervention for PTSD symptoms. However, this study also has some limitations. First, it failed to use a good innovative experimental design to reduce the non-specific effects of TMS and similar studies with large sample sizes are needed. The second is the accuracy of target positioning. This study used the "standard 10–20 EEG system" and "hot spot of hand motion" rule positioning. Some studies have shown that this may be a suboptimal method and may not find the best treatment position for all patients. With the help of brain imaging navigation technology, the target can be accurately located. Third, no biomarkers or other biological aspects were included, which would help understand exactly why TMS is important for PTSD symptoms. Fourth, the study did not combine TMS with inducing PTSD symptoms, which may have resulted in suboptimal overall efficacy. Fifth, this study did not use a deep stimulation coil. Given the enhanced functional connectivity between the amygdala and hippocampus, use of a depth stimulation coil could directly modulate regions such as the amygdala by creating functional connections, which could enhance fear extinction. Overall this study provides new evidence for TMS in the treatment of post-traumatic stress disorder development. Future studies are needed to further elucidate mechanisms, optimize parameters, and explore the therapeutic potential and efficacy of iTBS in PTSD.

1.This content is organized by the Clinical Support Department of Shenzhen Yingchi Technology Co.,Ltd. Criticisms and corrections are welcome. For reprint, please indicate the source.
2.Reference: Yuan, H., Liu, B., Li, F., Jin, Y., Zheng, S., Ma, Z., Wu, Z., Chen, C., Zhang, L., Gu, Y., Gao, X., & Yang, Q. (2023). Effects of intermittent theta-burst transcranial magnetic stimulation on post-traumatic stress disorder symptoms: A randomized controlled trial. Psychiatry research, 329, 115533. https://doi.org/10.1016/j.psychres.2023.115533