Release time :2023-02-09
Source:support@yingchitech.com
Scan:1400
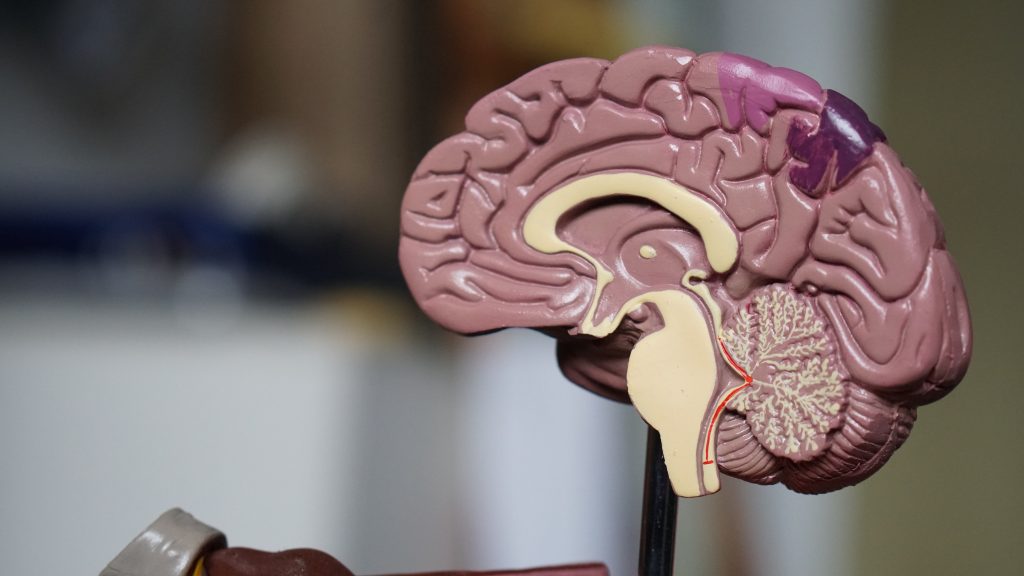
TMS is a non-invasive, safe, and painless brain stimulation technology. TMS principle is based on the Faraday’s Law, where a magnetic field was produce by the current of TMS coil, generating an induced current in and the targeted area of brain.
Diseases of neurology pathologically affect the integrity of our central and peripheral nervous system. That is, they will cause different damage and injury to the brain, spinal cord, cranial and peripheral nerve set, nerve roots of the autonomic nervous system and neuromuscular junctions:
......
For different treatment protocols, the target selection is based on the symptom and and characteristic of neurological disease. For example, to treat motor dysfunction caused by stroke or Alzheimer disease, the preferred target area is primary motor cortex. And to treat depression caused by neurological disease, the best intervention target is DLPFC, dorsolateral prefrontal cortex. It is a common site of stimulation for neurophysiological, cognitive, and mood.
Here are some TMS application in neurology fields.
Disorders of consciousness (DOC) mainly include minimally conscious state (MCS) and the “vegetative state,” clinically known as the unresponsive wakefulness syndrome (UWS). Normally,high frequency TMS protocols are adopted to treat DOC. The stimulation target are the left and right DLPFC, M1. iTBS protocol is also an available option for improving cognitive function and weakness. Although there is no recommendation for therapeutic use of TMS in DOC for now, some clinical benefit in consciousness obtained through the use of TMS protocols. The number of studies utilizing TMS in DOC patients continually expands, yet not all institutions are able perform the large, randomized controlled trials necessary to improve the level of evidence for therapeutic TMS. However the effect of TMS treating DOC cannot be overlooked.
Although antiepileptic drugs (AEDs) are the mainstay of epilepsy treatment, one third of patients on AEDs develop drug resistance. Under such circumstances, TMS technology could be a potential non-invasive treatment for the management of refractory epilepsy, as an alternative to epilepsy surgery. 1Hz rTMS therapy is safe and effective for improving cognitive function in patients with craniocerebral injury, and its mechanism may be related to rTMS reducing secondary damage, regulating neurotransmitters, affecting neuronal excitability, and achieving long-term cortical plasticity.
The rationale for using rTMS to suppress seizures in real time relates to its potential to interrupt synaptic potential and focal cortical excitability. The main concern for TMS is that in epileptic populations, it may actually cause seizures, although the chance inducing epilepsy is very small. The mechanism for treating Epilepsy are to reduce cortical hyper excitability associated with various epilepsy cortex .
TMS has been used to probe cortical excitability in various epilepsy syndromes, to assess the effects of antiepileptic drugs on the brain. While TMS was safe with no clear significant adverse events, the efficacy of rTMS for seizure reduction was lacking, despite rTMS reducing epileptiform discharges. There was too much variability in the studies regarding TMS techniques and outcome reporting.
Stroke rehabilitation for aphasia and motor function are 2 TMS focusing research fields. After stroke, a variety of neuroplastic changes occurs that may lead to decreased excitability of lesioned or perilesional brain regions and increased excitability of the homotopic regions in the contralateral hemisphere. This imbalance is believed to be maladaptive and primarily mediated by abnormally increased interhemispheric inhibition from the unaffected to the affected side. TMS stroke rehabilitation strategies aim to restore this disequilibrium via two main approaches: (i) increase cortical excitability of the affected hemisphere (for example, using high-frequency rTMS) or (ii) decrease cortical excitability of the contralateral hemisphere.
Normally, the low frequency of 1Hz or 0.5 Hz is adopted to treat stroke in perilesional brain areas, decreasing the excitability of such brain area.

Protocols of rTMS are based on persistently enhancing cortical excitability by repetitive high-frequency stimulation. Long-term potentiation (LTP)-like changes in synaptic strength, which are commonly assumed to be a major cellular mechanism of learning and memory. The expression of plasticity-related neurotrophins like brain-derived neurotrophic factor (BDNF) which diminishes in the hippocampus of Alzheimer's disease patients, is regulated by neuronal activity and LTP. Hence rTMS can considerably increase BDNF levels. By the correction or blunting of impaired LTP-like plasticity and associated signaling defects seen in AD, rTMS may provide clinical benefit. rTMS has also shown to be an inhibitory neuron function modifier which GABAergic synaptic strength on principal neurons is reduced by 10 Hz stimulation.For patients with mild to moderate AD, 20-Hz rTMS applied to the left and right DLPFC was found to improve cognitive function. Significant improvements were observed on cognitive abilities and daily activities.
MS is usually treated with disease-modifying therapies. However, despite treatment, patients develop relapsing/remitting MS (RRMS) and secondary progressing MS (SPMS). Since TMS has no known interaction with MS drugs, it can be used as an adjunctive treatment for management of motor and sensory symptoms of MS. It is believed that some of the MS symptoms are related to neuronal transmissionin the brain. LF-rTMS of a single neuron can cause prolonged inhibition of neuronal transmission while HF-rTMS can improve neuronal transmission. rTMS pulses could modify brain activity in the targeted region of brain lasting for minutes or even hours. Thus, TMS may alleviate debilitating Multiple Sclerosis symptoms such as fatigue, spasticity, and gait abnormalities and manual dexterity, which affect quality of life.
TMS and other types of non-invasive brain stimulation have not shown significantly clear or statistically strong data to support its use in the area of chronic pain. And there is no guidelines or consensus that support the TMS application in chronic pain. However, some study find that transient pain reduction could be achieved by applying high-frequency rTMS over the motor cortex corresponding to the painful area. The area could be mapped and confirmed by recording motor-evoked potentials the muscles of the affected areas.